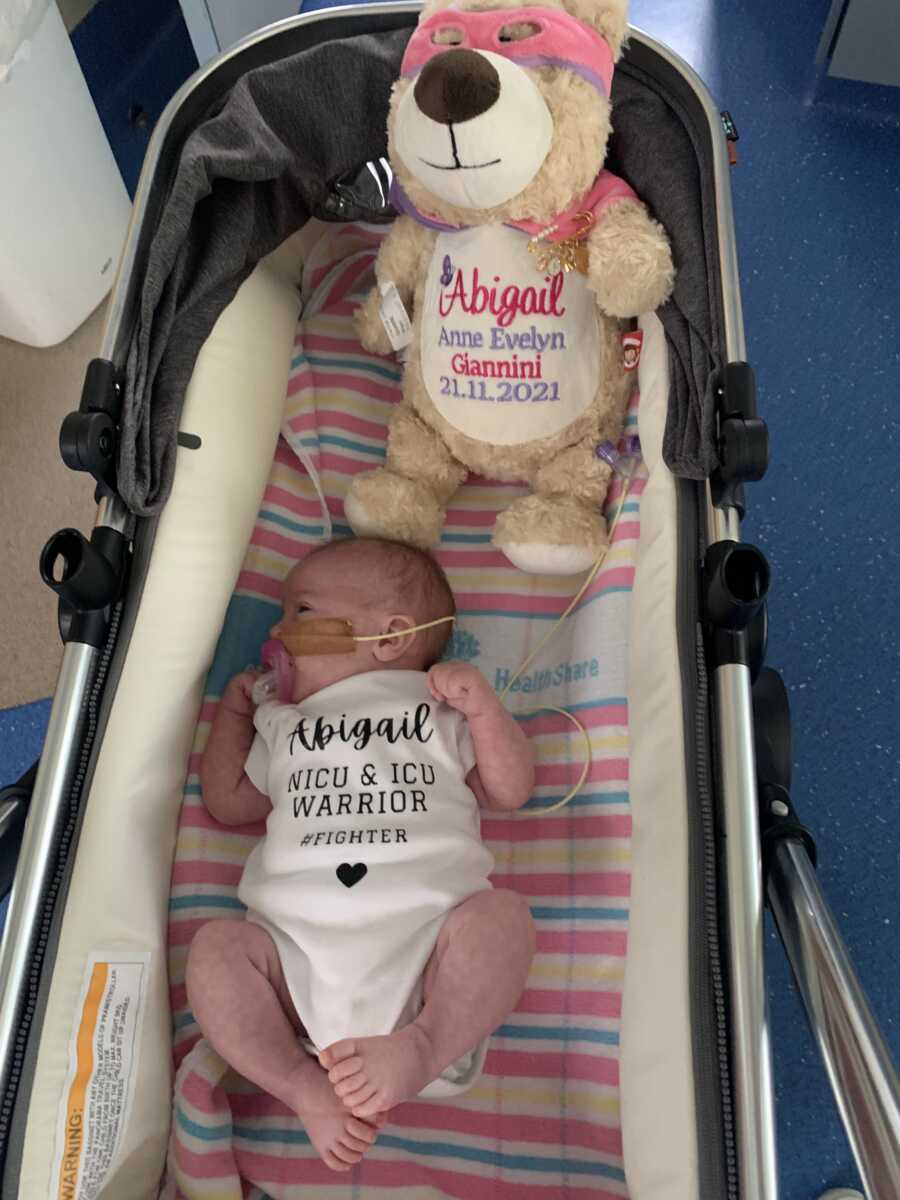
Our Little Miracle
“Our beautiful Abigail was born on November 21st, 2021, and is our beautiful IVF baby. Having been diagnosed with Endometriosis at age 16, I struggled to get pregnant and my husband and I decided to commence IVF in February 2021.
Against all odds (and only having two viable embryos) our first round was a success and we found out we were having our beautiful girl. I had a fairly normal pregnancy; all required screening tests came back nil to low risk. I was diagnosed with high blood pressure early in the pregnancy, however, at my 20-week scan, it was detected that Abigail had an issue with her heart. We were promptly sent to a cardiologist at the children’s hospital for investigation but to our relief, the condition that Abigail had was minor in the scheme of things. Whilst she needed to be monitored, we were assured there was only a small percentage this would affect Abigail later in life. So, overall, a normal pregnancy.
 Courtesy of Adrienne Giannini The Beginning Of Problems
Courtesy of Adrienne Giannini The Beginning Of Problems
As we progressed toward Abigail’s due date, her growth rate slowed down. I was monitored with scans closely and was told that Abigail was at risk of IUGR (intrauterine growth restriction) and the fact that I had high blood pressure meant we booked an induction date of November 20th, 2021. Our induction failed and after 12 hours with no progression, I was rushed into an emergency C-Section; Abigail had started to become quite stressed. When Abigail was born, she was very unwell and was taken straight from the table to special care and then moved to NICU. Abigail was hypoglycemic at birth and required to be placed on a ventilator on day 3 of her life for 48 hours. She was diagnosed with late-onset sepsis but thankfully progressed towards coming home. Three weeks after she was born, she was discharged on December 15th and we settled in as a family of 3.
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
Abigail had been really sleepy and not feeding well. She was very cold, mottled, and still quite jaundiced. Despite being a month old, she hadn’t moved past being 5.9 pounds (she was 6.1 pounds at birth). She wasn’t gaining enough weight, which again was put down to her having a rough start. We had a follow-up appointment with our pediatrician as she had been in the NICU on December 21st and we’d had the discussion that if she continued to not put on weight (also factoring in her being unwell at birth), we would do further investigations after Christmas. We got through Christmas and I had decided to start mix-feeding her to assist with weight gain.
On December 27th, I commenced mix feeding her one bottle; she’d taken in a decent amount and I thought we had turned a corner. Her bowel movements had started to change but I put that down to introducing formula. Until we began to notice she hadn’t been interested in eating as much the next day and on December 29th. That’s when everything changed. Our whole world changed.
Abigail hardly slept that night; it was the type of night where you feel like you’ve been awake every single second. As soon as we put her down, she would scream. I got up, my husband got up, and we tag-teamed trying to figure out what was wrong. She was only taking 10mls at a time from her bottle and falling back asleep. I remember sitting on the couch at 3 a.m. trying everything, watching Big Bang Theory in tears not knowing what was wrong with her. I decided I’d take candid photos holding her trying to find any positive of being so tired. My husband took over at 6 a.m. so I could get some sleep, as we had a family get-together for Christmas. I remember waking up at 11 a.m. and he told me she’d only had a total of 160mls of milk (which wasn’t enough).
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
We’d gone out for the day and she was still sleeping and refusing the bottle. I came up with a bunch of different reasons as to what was wrong. In my mind, I was able to justify that she was sleepier because we’d had a rough night. She wasn’t drinking because she didn’t feel like it. Maybe I had the incorrect bottle? It then suddenly hit me that she had been taking more when we had given her a particular brand of bottle. I thought I had found the solution and on the way home we stopped in at the baby store and I bought new bottles to try.
She started crying on the way home, so I rang my husband to quickly heat up the bottle and have it ready. Again, she refused, and I sobbed on the couch. My parents happened to be with us and I just cried and cried, feeling like a failure. I knew Abigail was now at risk of dehydration, but we decided to give her a little longer to have her milk. We put her in her bassinet to play and suddenly she went quiet. We heard this strange lip-smacking sound and as I reached her. We saw her having a seizure in front of my husband, myself, and my parents.
My dad swiftly picked her up because, at that point, we weren’t aware it was a seizure. Dad was convinced she was jerking from the hiccups, and I know he struggles with the fact he didn’t realize it was a seizure straight away. We watched, not knowing, and I suddenly saw my mom tap the back of my dad. Ever-so-subtly so I didn’t see it. But I did. Abigail had started turning blue in the lips so we called the ambulance. At this point, every fear I had since Abigail had come home was coming true. All those 3 a.m. thoughts. I threw the phone at my Dad and my husband and I started to gather everything I possibly could.
My husband Aaron and Dad had her in the recovery position on the tiles timing each breath. Once the paramedics arrived, she had stopped seizing. However, her blood sugar was 0.8, which meant she was severely hypoglycemic. As she stopped seizing, the critical care ambulance was canceled and they confirmed that we did wish to take her to the hospital for investigation. (Now, keep in mind that the end of December 2021 was when there was a sudden outbreak of Covid-19 cases in Australia. There were delays everywhere.)
 Courtesy of Adrienne Giannini Our Hardest Days
Courtesy of Adrienne Giannini Our Hardest Days
Due to Covid, I was the only parent allowed to go to the hospital. We didn’t know how long I’d be gone, so we kissed hubby goodbye and loaded her into the ambulance. The paramedics tried to feed Abigail her bottle which again had no response and attempted to give her oral glucose. In route to the hospital, Abigail became unresponsive and a code blue was issued for our arrival.
I can picture the moment they called the code. I drive past this road almost every day, and every day I can hear the same sounds. When Abigail and I were wheeled into the resuscitation bay, there was a team of around 20-30 doctors and nurses who promptly took Abigail out of my arms and commenced working on her. They cut her clothes off and tried to find out what was causing her to be so ill. The nurses started asking me all sorts of questions like, ‘Has anyone given her anything? Has she ingested a poison?’
In the background of it all, my daughter was unresponsive. Cannula after cannula was attempted with nothing working because of how dehydrated she was. One nurse grabbed me and told me they were about to attempt an intraosseous cannula where they drill into the bone to access and give fluid. She held my shoulders and told me to focus on her, that I didn’t want to watch. I did. I heard the drill go into her leg and not get anything. Then the other leg. Bingo. We had one cannula in to start fluids and antibiotics. Abigail needed assistance to breathe so at any chance I got (without being in the way), I’d go to her bedside and plead with her to wake up and breathe on her own. That her journey wasn’t over yet. That I needed my baby. I was alone.
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
There was a wonderful team on that night but in particular. A pediatric Doctor who ensured my husband was on the phone for any conversation that needed extra support. We knew at this point Abigail was Hypoglycemic (low blood sugar), Hypotensive (low blood pressure), and Hypothermic (a body temperature of only 84 degrees). We were told that Abigail’s pupils were fixed and dilated and she was in organ failure. They didn’t know why. Abigail was placed on life support and moved to Sydney Children’s Hospital at midnight after finally being stable enough for movement and they were instructed to have lights and sirens. It was time-critical.
At this point, I was numb; I hadn’t slept in what felt like forever. I was exclusively pumping for Abigail and hadn’t done so in almost 12 hours. We arrived at the Children’s Hospital and the handover was completed. The wonderful team said to me that I needed to sleep and get myself together as when we returned it would be one of the hardest days. She was critical but stable; there was nothing I could do. At 2 a.m. both my husband and parents pulled up at the hospital. It was cold and I fell into my mom’s arms in hysterics. It was the first time I had broken that night once I knew how serious it was. But I knew if I started crying, I wouldn’t stop. Aaron and I climbed into bed at 4 a.m. after checking she was still stable, and attempted to sleep.
I tried to prepare Aaron for how Abigail would look when we arrived at the hospital. He had already seen her quite unwell. But this was worse than we could have ever imagined. We walked in holding hands and started meeting with different teams to find an answer. What was wrong with our baby? Our first investigation was genetics. We spent close to two hours with the genetics team trying to trace family trees and genetic diseases that may be causing this. As we sat in that room with the genetics counselor, suddenly I wondered if we should have done extra testing on our embryo. We had no reason to, but suddenly I was faced with something that I may have regretted for the rest of our lives. They cross-checked all the medications I was on for my Psoriatic Arthritis. Again, guilt. I’d been reassured they were all safe, so I sat there quietly wondering if this was my fault? Thankfully, they were all fine.
 Courtesy of Adrienne Giannini The Road To Diagnosis
Courtesy of Adrienne Giannini The Road To Diagnosis
Abigail was stable. Neurology reassured us there was brain function, but were unsure as to what challenges we’d be faced with if or when she woke up. She was carrying a lot of fluid and showing different symptoms, but wasn’t assisting the doctors in getting a diagnosis. She’d check certain boxes for one condition, but not all. We’d move on to another. It was now New Year’s Eve. Our first New Year’s as a family and we couldn’t be together. In fact, we didn’t even know if she’d make it into the New Year, let alone what would happen. We rang the ICU at midnight and asked the doctor to put the phone to Abigail’s ear so we could wish her a Happy New Year and only hope that the next would be better.
Days into 2022, Abigail slowly started responding to treatment. They continued to rule out certain conditions. We looked into different cancers, infections, and obvious answers, but we still had no concrete answer. We sat there almost hoping each time it would be that particular issue so that we could at least deal with it. She had slowly started to wake up and move. Then, suddenly, she started responding to her name. Started moving all four limbs. Little things that gave me hope for her neurological function despite the poor outlook. Towards January 10th, whilst Abigail was still on life support, she was taken for an MRI. She’d had one in NICU but was not sedated so she had moved. This time they were able to get a clearer picture. We got the call the Saturday morning letting us know that the MRI had shown that her Pituitary Gland had appeared to be smaller than what they wanted.
The Answers
That Monday we had a meeting with the multidisciplinary teams and it was confirmed that Abigail was to be diagnosed with a condition called Hypopituitarism. Aaron had come across this condition days earlier when googling and together we breathed a sigh of relief that we finally had an answer. A scary and unknown future, but we had the answer.
Hypopituitarism is a rare disorder in which your pituitary gland fails to produce one or more hormones, or doesn’t produce enough hormones. The pituitary gland is a kidney-bean-sized gland situated at the base of your brain. Abigail was producing little to none of the hormones Cortisol, Growth Hormone, and Thyroid Hormone. We then started to learn more about what had in fact made Abigail so unwell, and it was that she had an Adrenal crisis due to Adrenal Insufficiency.
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
Adrenal Insufficiency ‘AI’ occurs when the body is unable to produce enough Cortisol. Cortisol helps maintain the body’s functions such as blood pressure, heart muscle tone, sugar, salt balance, and more. Just as a diabetic takes insulin to live, those with ‘AI’ must take cortisol replacements multiple times a day to live. An Adrenal crisis can lead to shock, heart failure, disability, and even death. During times of illness and injury, the body naturally produces up to 10x of the normal amount of cortisol. The extra cortisol is needed because the body must work harder to maintain its normal functions until the illness has passed or the injury has been treated.
Since Abigail cannot produce enough cortisol on her own to begin with, an additional dose of cortisol (referred to as a ‘stress dose’) must be given during illness and injury to prevent an adrenal crisis. Until her cortisol levels are increased so her body is able to maintain its own functions, no other treatment will be effective. Depending on the type of illness and/or injury, Abigail receives a stress dose via extra Hydrocortisone tablets and/or injection.
 Courtesy of Adrienne Giannini Another Layer
Courtesy of Adrienne Giannini Another Layer
My husband and I were suddenly needing to become masters in a condition we’d never heard of. In the midst of learning about the condition, the Genetics team had confirmed there was a gene variant in Abigail that can cause Hypopituitarism. However, only one copy of that gene was not working, which they had not come across before. As I type, we are still doing ongoing genetic testing.
Our job as parents is to now replace those missing levels of critical hormones to ensure Abigail stays a healthy baby, child, and then adult. Abigail is given her growth hormone every single night, administered by us and will continue to do so for the rest of her life. The dose will change as she grows and becomes older, but to ensure she does (essentially) grow, she will need to continue this. When Abigail hits puberty, we will also have to commence sex hormones to ensure the puberty process commences as it would for others. She is also on Thyroid medication to ensure her thyroid continues to function ‘normally’ and as previously mentioned Cortisol replacements.
There are so many variables with knowing when we need to stress dose Abigail with extra Cortisol. We have a guide for certain scenarios of when it would be appropriate to increase, but we are learning and essentially trusting our gut feeling that it is the correct choice. As Abigail becomes older, this will be easier. She will be able to say, ‘Mom and Dad, I don’t feel well,’ but at the moment, she is just a baby. Is she just being a normal fussy baby? Is she feeling unwell? Do I need to stress dose? This is the mental load I carry each day.
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
On the outside, Abigail appears and looks like any other baby. She is on the smaller side and still has a feeding tube to assist her (which will hopefully be gone soon!). You wouldn’t know that she had been so critically unwell. Whilst becoming new parents for the first time, we’ve had to face challenges we never thought were possible. It has made us stronger as a family, but it is also very tiring. We are now Abigail’s greatest advocates so we can be her voice and continue to raise awareness.
We’ve mourned as a family; Abigail was in the hospital essentially for the first three months of her life. We missed the newborn stage. We’ve questioned why this has happened to her, what did she ever do to be given this challenge at such a young age? Will she feel normal? Does she understand that we inject her with her Growth Hormone to help her? Will she recognize her own symptoms? Will she ever have an adrenal crisis like that again?
But we’ve also learned that no matter the challenge, this girl has a purpose. And we are so incredibly lucky to have her here; every day we are thankful. We are so incredibly proud of her and also thankful every day for those who helped to save her.”
 Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini  Courtesy of Adrienne Giannini
Courtesy of Adrienne Giannini
This story was submitted to Love What Matters by Adrienne Giannini from Sydney, Australia. You can follow her journey on Instagram and her blog. Submit your own story here. Be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more inspiring stories like this:
‘Through screaming, I coded at 1:25 p.m. 5 minutes later, my son was born not breathing. He was bagged and taken for CPR.’: Mom births baby with rare apert syndrome
‘After I delivered, my doctor handed me my girl. I did not see it. In all of my medical training, I could not tell. She was the most beautiful baby I had ever seen. She was PERFECT.’
‘I was suddenly watching her monitor flat-line. Countless nurses rushed to save her. It happened 20 times that day.’: Mother shares traumatic process diagnosing daughter with Adrenal Insufficiency
‘My hands were shaking as I gripped my son’s tiny hand in the backseat. ‘Just hurry up and get to the hospital.’: Mom’s confusion after ‘idyllic’ newborn’s rare Congenital Adrenal Hyperplasia diagnosis
Do you know someone who could benefit from this story? Please SHARE on Facebook or Twitter
192 Shares Tweet Email adrenal insufficiency, endometriosis, Hypopituitarism, IVF, rare disease, sepsis ‘The doctor described it as a ‘stress fracture’ but a mental one. She had hit her breaking point.’: Mother shares daughter’s journey with Tourette Syndrome‘I have a 13-year-old daughter most people only think about twice a year — the day she was born and the day she died.’: Mom shares raw grief on anniversary of daughter’s passing
Source: lovewhatmatters.com